Body Mass Index has dominated health assessments for decades, yet mounting evidence suggests this widely-used metric may be fundamentally flawed.
While BMI continues to serve as a primary screening tool in medical settings worldwide, health professionals increasingly question whether a simple height-to-weight ratio can accurately reflect individual health status.
The growing debate surrounding BMI accuracy stems from its inability to account for crucial factors that significantly impact health outcomes.
Modern research reveals that body composition, muscle mass distribution, and genetic variations play far more complex roles in determining health risks than BMI calculations can capture.
Understanding BMI’s limitations becomes essential as healthcare moves toward more personalized, comprehensive assessment approaches. This critical examination explores why BMI might not tell the full story about your health and what alternatives offer more accurate insights.
The Core Criticisms of BMI
BMI’s fundamental flaw lies in its oversimplification of human physiology. By reducing health assessment to a mathematical relationship between weight and height, BMI ignores the complex interplay of factors that determine actual health status and disease risk.
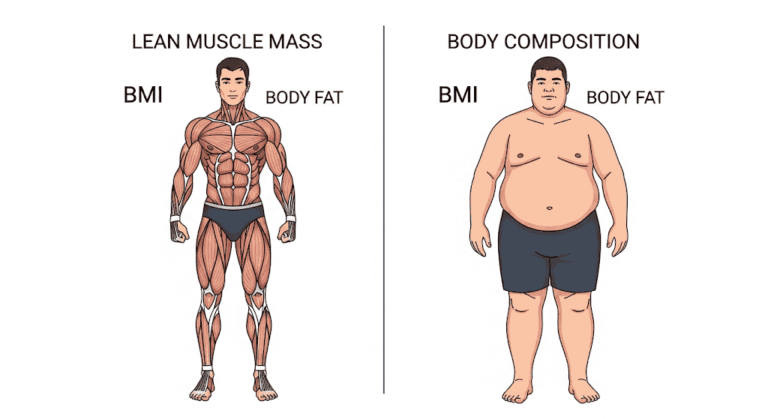
The most significant oversight involves BMI’s inability to distinguish between different types of body mass. Two individuals with identical BMI scores can have vastly different body compositions one might carry excess fat tissue while the other possesses high muscle mass.
This distinction proves crucial since muscle tissue and fat tissue have completely different metabolic profiles and health implications.
Muscle mass represents metabolically active tissue that burns calories, supports bone health, and contributes to overall strength and mobility.
Conversely, excess adipose tissue, particularly visceral fat, increases inflammation and disease risk. BMI treats these tissue types identically, creating fundamentally inaccurate health assessments.
Body fat distribution presents another critical limitation. Research consistently demonstrates that fat location matters more than total amount.
Visceral fat surrounding internal organs poses significantly higher health risks than subcutaneous fat stored beneath the skin.
Yet BMI cannot differentiate between these distinct fat distribution patterns, potentially misclassifying individuals with dangerous visceral adiposity as healthy while flagging those with benign subcutaneous fat storage.
Bone density variations further complicate BMI accuracy. Individuals with dense, heavy bones may register higher BMI values despite having optimal body composition.
This biological variation means BMI can misclassify people with naturally heavy skeletal structures as overweight or obese when their actual health status remains excellent.
Health professionals increasingly express concern that BMI serves as too blunt an instrument for meaningful health assessment. The metric’s binary approach categorizing individuals as underweight, normal, overweight, or obese fails to capture the nuanced reality of human physiology and health risk factors.
When BMI Fails to Reflect Reality
Athletes and Muscular Individuals
BMI demonstrates its most glaring inadequacies when applied to athletes and individuals with above-average muscle mass. Professional athletes routinely register BMI values in the overweight or obese categories despite possessing exceptionally low body fat percentages and superior cardiovascular health.
Studies examining NFL players reveal that over 95% would be classified as overweight or obese based on BMI, despite body fat percentages often below 10%.
These individuals possess extensive muscle development that dramatically increases their weight relative to height, triggering BMI misclassification despite optimal health markers.
Research published in the International Journal of Obesity found that BMI misclassified 25% of men and 48% of women when compared to direct body fat measurements.
The study revealed that many individuals classified as “normal weight” actually carried excess body fat, while others labeled “overweight” possessed healthy body compositions with higher muscle mass.
Strength athletes, bodybuilders, and individuals engaged in resistance training frequently encounter BMI inaccuracies.
Their developed musculature can push BMI values well into obese ranges while maintaining single-digit body fat percentages.
This misclassification can lead to inappropriate medical recommendations and insurance complications based on fundamentally flawed assessments.
Older Adults and Sarcopenia
BMI’s limitations become particularly pronounced in elderly populations, where age-related muscle loss (sarcopenia) significantly impacts body composition.
Older adults may maintain stable BMI values while experiencing dramatic shifts in muscle-to-fat ratios that substantially increase health risks.
Sarcopenia affects approximately 10% of adults over 60, with prevalence increasing dramatically with age. This condition involves progressive muscle mass loss accompanied by strength decline and functional impairment.
However, BMI cannot detect sarcopenia since lost muscle mass is often replaced by fat tissue, maintaining similar overall weight.
Research demonstrates that older adults with “normal” BMI values frequently harbor dangerous levels of visceral fat while lacking adequate muscle mass for mobility and metabolic health.
This phenomenon, termed “sarcopenic obesity,” represents a high-risk health condition that BMI fails to identify.
Studies following elderly populations reveal that slightly higher BMI values (traditionally classified as “overweight”) often correlate with better health outcomes and longevity.
This “obesity paradox” suggests that BMI thresholds established for younger populations may be inappropriate for older adults, whose nutritional and metabolic needs differ significantly.
People with Unique Body Types
BMI’s one-size-fits-all approach fails to accommodate natural variations in human body structure. Tall individuals often register artificially low BMI values due to the squared height component in BMI calculations, while shorter individuals may appear to have elevated BMI despite healthy body compositions.
The mathematical relationship between height and weight doesn’t scale linearly, creating systematic biases in BMI calculations.
Very tall individuals require proportionally more weight to achieve the same BMI as shorter people, potentially masking underweight conditions or creating unrealistic weight targets.
Individuals with naturally dense bone structures face similar challenges. Bone mineral density varies significantly among populations and individuals, with some people possessing naturally heavy skeletal frameworks.
These individuals may register higher BMI values despite having optimal muscle and fat distributions.
Body frame size whether small, medium, or large significantly impacts appropriate weight ranges for health. BMI calculations ignore these natural variations, potentially misclassifying individuals whose weight falls within healthy ranges for their specific body structure.
Cultural and Genetic Limitations of BMI
BMI’s universal application across diverse populations reveals significant cultural and genetic limitations that undermine its accuracy for specific ethnic groups.
Research demonstrates that BMI thresholds established primarily from Caucasian populations may be inappropriate for other ethnicities with different body composition patterns and disease risk profiles.
The World Health Organization has acknowledged these limitations by recommending lower BMI thresholds for Asian populations.
Asian individuals typically develop obesity-related health complications at lower BMI values than Caucasians, suggesting that standard BMI categories underestimate health risks in these populations.
Studies examining Asian populations reveal increased diabetes and cardiovascular disease risks at BMI values traditionally considered “normal” for Western populations.
This finding has led to revised BMI thresholds: overweight at 23 kg/m² and obesity at 25 kg/m² for many Asian countries, compared to standard thresholds of 25 and 30 kg/m².
African American populations demonstrate opposite patterns, with higher BMI values often associated with lower health risks compared to Caucasians.
Research indicates that African Americans typically possess greater muscle mass and bone density, leading to higher BMI values without corresponding increases in body fat or health complications.
Genetic predispositions significantly influence body fat distribution patterns, with some populations more prone to visceral fat accumulation while others predominantly store subcutaneous fat.
These distribution differences dramatically impact health outcomes despite similar BMI values, highlighting the metric’s inability to account for genetic variations.
Hispanic populations show unique patterns of fat distribution and metabolic health that don’t align with standard BMI categories.
Research reveals that genetic factors influence where fat is stored and how it impacts metabolic function, creating population-specific risk profiles that BMI cannot capture.
The application of universal BMI standards raises important equity concerns in healthcare. Using inappropriate thresholds for specific populations can lead to delayed diagnosis of obesity-related conditions in some groups while creating unnecessary alarm in others. This systematic bias undermines the goal of equitable healthcare delivery.
Expert Opinions on the Future of BMI
Leading health professionals increasingly advocate for comprehensive assessment approaches that extend beyond BMI’s limitations.
Dr. Fatima Cody Stanford, an obesity medicine specialist at Massachusetts General Hospital, emphasizes that “BMI is a starting point, not an endpoint” in health evaluation.
The American Medical Association has formally recognized BMI’s limitations, stating that it should be used alongside other measurements rather than as a standalone diagnostic tool.
This position reflects growing professional consensus that comprehensive health assessment requires multiple metrics.
Nutritionists and registered dietitians frequently encounter BMI’s practical limitations in clinical practice. Many report that clients with “normal” BMI values struggle with metabolic health issues, while others classified as “overweight” demonstrate excellent health markers across multiple parameters.
Research institutions are developing alternative metrics that address BMI’s shortcomings. Body fat percentage provides more accurate health assessment by directly measuring adipose tissue rather than inferring it from height and weight relationships.
However, body fat measurement requires specialized equipment and training, limiting its practical application.
Waist-to-hip ratio offers another alternative that better reflects fat distribution patterns. This metric specifically identifies dangerous visceral fat accumulation that BMI cannot detect. Studies demonstrate stronger correlations between waist-to-hip ratio and health outcomes compared to BMI alone.
DEXA scans represent the gold standard for body composition analysis, providing detailed measurements of muscle mass, bone density, and fat distribution. While expensive and requiring specialized equipment, DEXA scans offer comprehensive insights that BMI cannot provide.
Bioelectrical impedance analysis (BIA) presents a more accessible alternative, using electrical conductivity to estimate body composition.
Though less accurate than DEXA scans, BIA provides valuable information about muscle and fat distribution that improves upon BMI’s limitations.
Many experts advocate for composite scoring systems that combine multiple metrics rather than relying on any single measurement.
These comprehensive approaches consider BMI alongside body fat percentage, waist circumference, and metabolic markers to provide more accurate health assessments.
The medical community increasingly recognizes that BMI retains value as a quick screening tool for population-level health surveillance. However, experts emphasize that individual health assessment requires more sophisticated approaches that account for the complex factors BMI ignores.
Conclusion: Should You Trust Your BMI Number?
BMI’s limitations don’t render it entirely useless, but they do highlight the need for more nuanced approaches to health assessment. The metric serves as a reasonable starting point for population-level health screening, but individual health decisions should incorporate additional factors that BMI cannot capture.
The fundamental issue isn’t that BMI is inherently “bad,” but rather that it’s incomplete. Like any screening tool, BMI provides limited information that requires context and professional interpretation. The danger lies in treating BMI as a definitive health assessment rather than one piece of a larger puzzle.
For most individuals, BMI can provide general guidance about weight status, but it shouldn’t be the sole determinant of health goals or medical decisions.
People with higher muscle mass, unique body types, or specific genetic backgrounds may find BMI particularly unhelpful or even misleading.
The future of health assessment likely involves personalized approaches that consider individual body composition, genetic factors, and metabolic health markers. As technology advances and becomes more accessible, comprehensive body composition analysis may eventually replace BMI as the standard screening tool.
Healthcare providers increasingly emphasize the importance of looking beyond BMI to assess overall health. Factors such as cardiovascular fitness, metabolic markers, strength, and functional capacity provide more meaningful insights into health status than BMI alone.
Rather than obsessing over BMI numbers, individuals should focus on sustainable healthy behaviors including regular physical activity, balanced nutrition, adequate sleep, and stress management. These lifestyle factors have proven health benefits regardless of BMI classification.
Professional guidance becomes essential when BMI seems inconsistent with other health indicators. Healthcare providers can perform comprehensive assessments that account for individual factors BMI cannot measure, providing more accurate and actionable health insights.
FAQs
Is BMI accurate for muscular people?
BMI is notoriously inaccurate for muscular individuals, frequently misclassifying them as overweight or obese despite having low body fat percentages and excellent health markers. Athletes and people with above-average muscle mass should compare BMI to body fat percentage for more accurate assessment.
Why is BMI not accurate for older adults?
BMI fails to account for age-related muscle loss (sarcopenia) and changes in body composition that occur with aging. Older adults may maintain stable BMI while experiencing dangerous shifts in muscle-to-fat ratios that significantly impact health outcomes.
Is BMI outdated?
While BMI isn’t entirely outdated, it’s increasingly recognized as insufficient for individual health assessment. The metric retains value for population-level health surveillance but requires supplementation with more comprehensive measures for accurate individual evaluation.
What are better alternatives to BMI?
Superior alternatives include body fat percentage, waist-to-hip ratio, DEXA scans, and bioelectrical impedance analysis. These methods provide more detailed information about body composition and fat distribution that BMI cannot capture.
Should athletes worry about high BMI?
Athletes with high BMI due to muscle mass shouldn’t be concerned if other health markers remain optimal. However, they should learn why BMI often misclassifies athletes and work with healthcare providers familiar with athletic populations for accurate assessment.
Does ethnicity affect BMI accuracy?
Yes, BMI accuracy varies significantly across ethnic groups. Some populations develop health complications at lower BMI values while others remain healthy at higher values, highlighting the need for population-specific thresholds.
If you’re curious about your BMI despite its limitations, you can calculate your BMI here while keeping in mind the factors discussed in this analysis.